AI and Digital Innovation in GCC Healthcare: Building System-Level Intelligence
Authored by: Nidhi Gupta, Principal Consultant, Healthcare & LifeSciences, Frost & Sullivan
Why does AI in healthcare matter for the GCC?
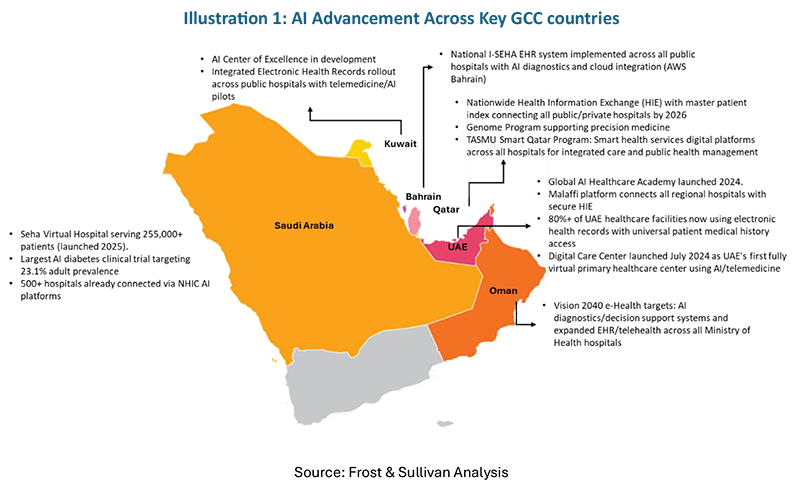
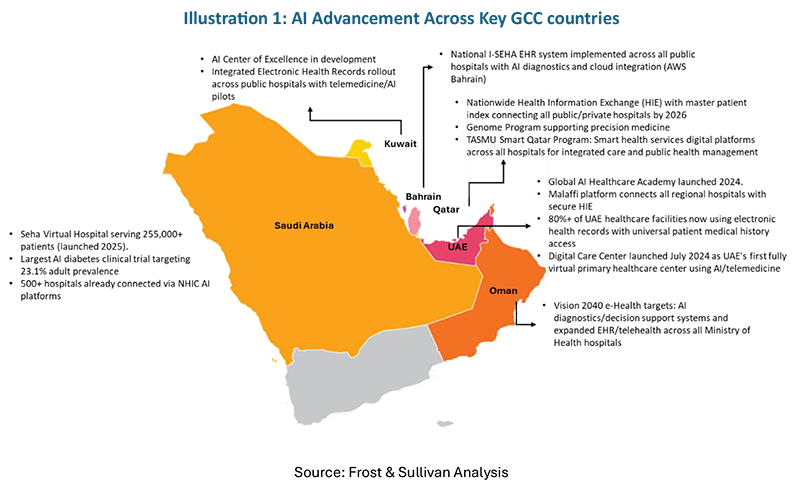
Healthcare in the GCC is being shaped by three powerful dynamics coming together: growing demand for care, an increased focus on managing chronic conditions, and a strong commitment by governments to ensure long-term cost sustainability.
Traditional care models rely on patients coming to hospitals, doctors working with limited data, and many manual steps in diagnosis and administration. This model is hard to scale when millions of people need regular monitoring and long-term treatment. AI and digital tools offer a different approach, i.e. using data to detect risk early, coordinate resources across the system, and free clinicians from routine work so they can focus on complex decisions and patient interactions.
A key difference in the GCC is that healthcare is largely government-funded and centrally planned. This means AI is not just being adopted hospital by hospital; instead, entire national platforms are being built, such as Seha Virtual Hospital (SVH) in Saudi Arabia and Malaffi in Abu Dhabi, that push digital and AI capabilities into routine care.
Three layers of AI in GCC healthcare
A simple way to understand AI in GCC healthcare is to look at three connected layers: intelligence inside clinical care, system-level orchestration, and patient engagement.
❖ Intelligence inside care delivery
A. In the GCC, AI is used in diagnostics and specialist workflows through AI-enabled imaging and remote diagnostics, such as at Saudi Arabia's Seha Virtual Hospital (SVH), where scans from 200+ connected hospitals are AI pre-screened, urgent abnormalities like strokes are flagged, and standardized remote specialist review is enabled via centralized digital platform.
B. AI-driven clinical decision support assists doctors in following treatment pathways and reducing medication errors. Saudi Arabia is also deploying AI-supported and robot-assisted surgery that uses imaging data and computer vision to guide procedures and improve surgical consistency.
C. Natural-language AI tools are used to generate clinical notes, support coding, and automate routine documentation
❖ Health System – level orchestration
A. At the system level, GCC countries—particularly Saudi Arabia—use AI analytics to stratify populations by chronic disease risk and guide large-scale screening and early intervention programs.
B. AI-enabled digital command centers integrate data from hospitals, primary care, virtual platforms, and public health systems to forecast bed occupancy, plan specialty capacity, and optimize use of diagnostic and clinical assets.
C. National platforms such as SVH and Malaffi provide integrated data that enables this AI-driven coordination. AI-powered surgical workflows are also used to predict operating times and support hospital scheduling and capacity planning
❖ Patient engagement and access
A. AI is used to deliver virtual care and remote monitoring, integrated with national health systems. Saudi Arabia’s Sehhaty app, which underpins much of the digital front door for the health system, facilitated over 51 million virtual consultations and appointments in 2024 and serves ~88% of the population. SVH connects hospitals to provide virtual specialist consultations, “hospital at home” services, and remote monitoring for chronic conditions.
B. In the UAE, health information exchanges such as Malaffi and NABIDH allow telehealth providers to access unified patient records, enabling AI-supported virtual care to function as part of continuous treatment pathways.
C. AI-driven virtual clinics are being piloted for first-line assessment, follow-ups, and chronic disease management.
Digital maturity: from data-enabled to data-driven
The GCC’s visible AI adoption rests on more than a decade of investment in basic digital infrastructure. Across the region, governments have rolled out national or regional electronic health record programs, interoperable hospital information systems, and foundational telehealth platforms. This has moved systems from simply digitizing paper processes to using data as a strategic asset for planning and care.
Why is AI scaling fast in the GCC?
AI adoption is accelerating in the GCC healthcare because structural conditions make it both necessary and scalable.
1. First, the region’s disease burden presents a significant economic and clinical opportunity. Recognizing this, Saudi Arabia and the UAE are proactively addressing the high prevalence of diabetes, cardiovascular disease, and obesity. AI enables early risk identification, population screening, and targeted intervention at scale, easing long-term pressure on hospitals.
2. Second, specialist capacity is not keeping pace with demand. Procedure volumes are rising—particularly in orthopedics, now the largest revenue segment in Saudi ambulatory surgery centers—driven by aging populations and higher musculoskeletal disease prevalence. AI-supported diagnostics, standardized pathways, and remote specialist oversight allow systems to absorb growth without proportionally increasing consultant headcount.
3. Third, centralized financing and regulation allow faster scale-up. Once AI-enabled diagnostics or robotic systems are approved by bodies such as the SFDA under Vision 2030, they can be deployed across national public-hospital networks with centralized procurement and reimbursement. Similarly, mandated participation in platforms like Malaffi enables system-wide analytics and AI use across nearly all providers in Abu Dhabi.
4. Fourth, relatively modern health IT reduces legacy friction. Many GCC providers have implemented standardized digital platforms within the last 10–15 years, making AI integration into core workflows easier than in systems constrained by decades-old infrastructure.
What enables AI deployment in practice?
AI scale-up is supported by six reinforcing enablers.
1. Data availability and governance: The GCC is building national health databases, disease registries, and genomics programs—particularly in Saudi Arabia, the UAE, and Bahrain—providing localized data for training and validation. Governance frameworks emphasize secure data sharing, sovereign cloud models, and defined public–private access rules.
2. Digital and physical infrastructure: Hospitals are being designed as smart facilities, with connected imaging, devices, and IoT systems feeding real-time data into command centers. Platforms such as Malaffi and Seha Virtual Hospital (SVH) support interoperability, enabling analytics for bed management, referrals, equipment use, and remote monitoring.
3. Regulatory readiness: Regulators have adopted approval pathways for AI-enabled software, diagnostics, and robotic systems. SFDA’s expedited frameworks under Vision 2030 balance speed with clinical safety, giving innovators a clear route from pilot to national rollout.
4. Global collaboration models: Global partnerships increasingly focus on co-development and localization. Abu Dhabi’s collaboration with Nvidia and Saudi Arabia’s AI-powered virtual care models anchored by SVH combine international technology with local data and workflows.
5. Capital and policy support: Capital and policy support reinforce momentum. Sovereign funds and national strategies—such as Saudi Arabia’s AI strategy and Qatar’s Digital Agenda 2030—direct funding and incentives toward digital health, AI, and biotech, reducing adoption risk.
6. Talent development: Talent development complements this, with investments in clinician upskilling, local data science capacity, and targeted immigration pathways for high-skill AI and health-tech professionals.
What comes next: AI as system infrastructure?
The next phase is less about new tools and more about embedding AI into how healthcare is planned and run. As SVH, Malaffi, and similar platforms mature, AI will increasingly shape decisions upstream—who is screened, how referrals flow, how operating lists and beds are allocated—before clinicians intervene.
Decision-making will continue shifting from individual hospitals to regional and national command centers, coordinating capacity and prioritization using near real-time data and predictive models. This improves consistency, cost control, and predictability across networks.
Clinical roles will adjust accordingly. Routine interpretation, documentation, and protocol-driven decisions will be AI-supported, while clinicians focus on complex cases, multi-morbidity, and patient communication. Given specialist constraints and rising volumes, this shift is structural rather than optional.
Over time, the accumulation of GCC-specific clinical, imaging, and genomic data will produce AI models that outperform imported ones for local populations. This turns population health data into a strategic asset—supporting better domestic care and positioning the GCC as an exporter of AI-enabled health system design.
Much of this change is already visible in daily practice. The deeper transformation will be quieter: AI operating in the background as core infrastructure, shaping how GCC healthcare systems are governed, scaled, and sustained.
DISCLAIMER
Frost & Sullivan is not responsible for any incorrect information supplied by companies or users. Quantitative market information is based primarily on interviews and therefore is subject to fluctuation. Frost & Sullivan research services are limited publications containing valuable market information provided to a select group of customers. Customers acknowledge, when ordering or downloading, that Frost & Sullivan research services are for internal use and not for general publication or disclosure to third parties. No part of this research service may be given, lent, resold, or disclosed to noncustomers without written permission. Furthermore, no part may be reproduced, stored in a retrieval system, or transmitted in any form or by any means—electronic, mechanical, photocopying, recording, or otherwise—without the permission of the publisher.
ABOUT FROST & SULLIVAN
YOUR TRANSFORMATIONAL GROWTH JOURNEY STARTS HERE
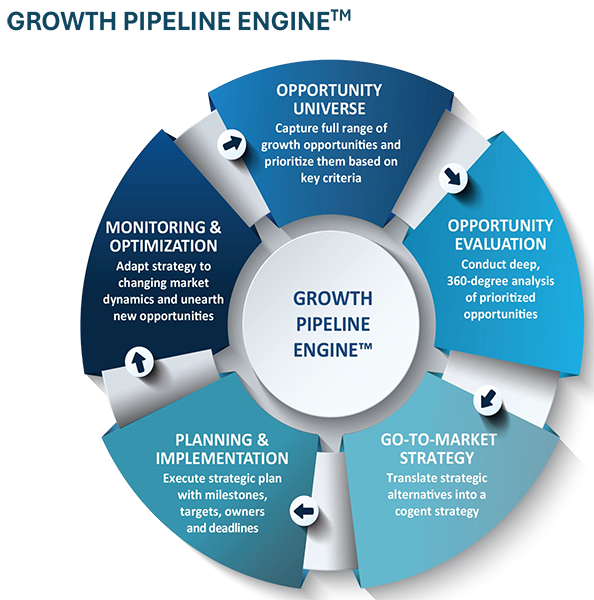
Frost & Sullivan’s Growth Pipeline Engine, transformational strategies and best-practice models drive the generation, evaluation, and implementation of powerful growth opportunities.
Is your company prepared to survive and thrive through the coming transformation?
Join the journey
To get in touch with our Growth Advisory Experts, E-mail: [email protected]
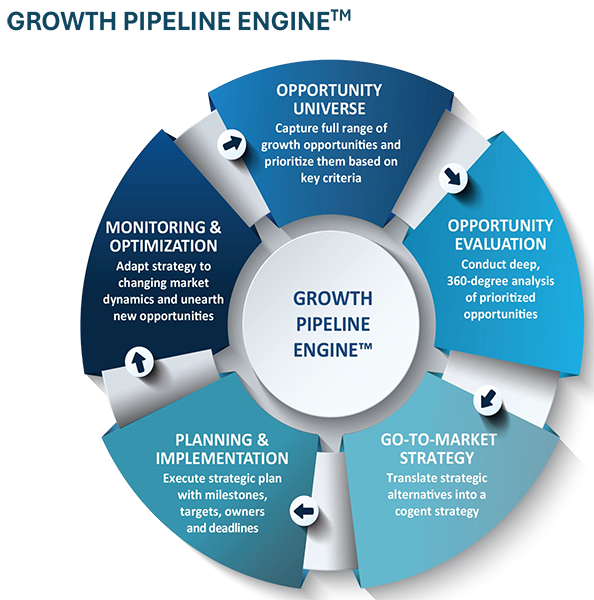
Frost & Sullivan’s Growth Pipeline Engine™ supports clients through all 5 phases of growth: from developing, evaluating, and prioritizing opportunities to building and implementing go-to-market strategies and optimizing opportunities. The objective of this study is to be a client’s first step on a growth journey.